A new study led by researchers at University College London (UCL) has found that pain is the most common and severe symptom reported by people suffering from long COVID.
This condition, which affects individuals long after their initial COVID-19 infection, includes a range of symptoms, but pain appears to be the most prevalent.
The study, published in JRSM Open, analyzed data from over 1,000 people in England and Wales who recorded their symptoms using an app between November 2020 and March 2022.
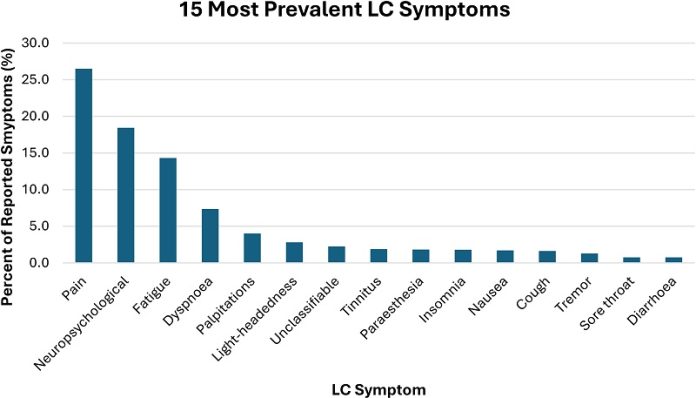
The results showed that 26.5% of participants experienced pain, including headaches, joint pain, and stomach pain, making it the dominant symptom among those with long COVID.
Other common symptoms reported were neuropsychological issues like anxiety and depression (18.4%), fatigue (14.3%), and shortness of breath (7.4%).
The study also found that the intensity of symptoms, particularly pain, increased over time, rising by an average of 3.3% each month after participants first registered their symptoms.
The researchers also explored how different demographic factors influenced the severity of symptoms.
Older individuals were found to suffer more severe symptoms, with those aged 68–77 experiencing 32.8% more intense symptoms, and those aged 78–87 facing an 86% increase in symptom severity compared to younger adults aged 18–27.
Gender also played a role, with women reporting 9.2% more intense symptoms, including pain, than men.
Additionally, ethnicity influenced symptom severity, as non-white participants reported 23.5% more intense symptoms compared to white participants.
The study revealed that education level had a significant impact on symptom severity as well. People with higher education qualifications experienced less severe symptoms.
For instance, those with NVQ level 3, 4, or 5 qualifications (equivalent to A-levels or higher education) reported a reduction in symptom severity of 27.7%, 62.8%, and 44.7%, respectively, compared to those with lower education levels (equivalent to GCSEs).
Socioeconomic status, measured by the Index of Multiple Deprivation (IMD), also affected symptom intensity.
Participants from less deprived areas reported less severe symptoms than those from more deprived areas.
However, the number of symptoms did not significantly differ based on socioeconomic status, suggesting that while deprivation may worsen symptom severity, it does not necessarily lead to a wider range of symptoms.
Dr. David Sunkersing, the lead author from UCL’s Institute of Health Informatics, emphasized the importance of these findings. “Our study highlights pain as the predominant symptom in long COVID, and it also shows how demographic factors play a significant role in symptom severity,” he said.
“As new COVID-19 variants emerge, the potential for more long COVID cases remains a concern. Our findings can help shape targeted interventions and support strategies for those most at risk.”
The researchers called for continued support for long COVID clinics and the development of treatment strategies that prioritize pain management.
They also stressed the need for health care policies that address the disparities in symptom severity, ensuring that all individuals affected by long COVID receive equitable care.
The study did have some limitations, including a lack of information on participants’ other health conditions and health history.
The researchers also noted that the study might have excluded people with very severe COVID or those unable to access the app due to technological or socioeconomic barriers.
If you care about COVID, please read studies about vitamin D deficiency linked to severe COVID-19, death, and how diets could help manage post-COVID syndrome.
For more health information, please see recent studies that low-sodium plant-based diets may prevent COVID-19 better, and results showing zinc could help reduce COVID-19 infection risk.





